Inoculation Centers in India:
DELHI
Yellow Fever Vaccination Centre
Airport Authority of India Quarters
T1 Building
Near Mahipalpur Fly Over
Ph : 011 - 2565 2129
Timings = 2-4PM (Registrations from 10AM, best to register early as it's only done in batches of 10..)
Day = Tue/Thu
Public Health Laboratory
Municipal Corporation, Town Hall, Alipur Road
Timings: Fri :1000 - 1200 hrs
Tel: 2397 2058
Dr. Ram Manohar Lohia Hospital. Room No. 11 & 12
Timings: Wed & Sat 1100 to 1230 hrs
Tel: 2336 5525
International Inoculation Center
Mandir Marg, New Delhi - 110001
Timings: Wed & Fri : 1330 to 1400 hrs
Tel: 2336 2284
CHENNAI
King Institute of Preventive Medicine, Guindy
Port Health Officer/ Assistant Port Health Officer/ Assistant Airport Health Officer Port Health Organization
COCHIN
Port Health Organization
GOA
Urban Health Centre, Panaji
HYDERABAD
Institute of Preventive Medicine
JAMNANAGAR
Irwin Hospital
KANDLA
Port Health Organization
KASAULI
Central Research Institute
KOLKATTA
All India Institute of Hygiene and Public Health
Health Organization, Dum Dum Airport
Port Health Organization
LUCKNOW
Balrampur Hospital
MARMUGAO
Port Health Organization
MUMBAI
Health Office
Mumbai Airport
Port Health Organization
Seamen Medical Examination Organization
Nav Bhawan
PORBANDER
Office of the Civil Surgeon
VISHAKHAPATNAM
Port Health Organization
All About Yellow Fever
INFECTIOUS AGENT
Yellow fever virus (YFV) is a single-stranded RNA virus that belongs to the genus Flavivirus.
MODE OF TRANSMISSION
Vectorborne transmission occurs via the bite of an infected mosquito, primarily Aedes or Haemagogus spp. Nonhuman and human primates are the main reservoirs of the virus, with anthroponotic (human-to-vector-to-human) transmission occurring. There are 3 transmission cycles for yellow fever: sylvatic (jungle), intermediate (savannah), and urban.
- The sylvatic (jungle) transmission cycle involves transmission of the virus between nonhuman primates and mosquito species found in the forest canopy. The virus is transmitted via mosquitoes from monkeys to humans when the humans encroach into the jungle during occupational or recreational activities.
- In Africa, an intermediate (savannah) cycle involves transmission of YFV from tree hole-breeding Aedes spp. to humans living or working in jungle border areas. In this cycle, the virus may be transmitted from monkeys to humans or from human to human via these mosquitoes.
- The urban transmission cycle involves transmission of the virus between humans and urban mosquitoes, primarily Aedes aegypti.
Humans infected with YFV experience the highest levels of viremia and can transmit the virus to mosquitoes shortly before onset of fever and for the first 3–5 days of illness. Given the high level of viremia, bloodborne transmission theoretically can occur via transfusion or needlesticks.
EPIDEMIOLOGY
Yellow fever occurs in sub-Saharan Africa and tropical South America, where it is endemic and intermittently epidemic (see Tables 3-21 and 3-22 for a list of countries with risk of YFV transmission). Most yellow fever disease in humans is due to sylvatic or intermediate transmission cycles. However, urban yellow fever occurs periodically in Africa and sporadically in the Americas. In Africa, natural immunity accumulates with age, and thus, infants and children are at highest risk for disease. In South America, yellow fever occurs most frequently in unimmunized young men who are exposed to mosquito vectors through their work in forested or transitional areas.
Table 3-21. Countries with risk of yellow fever virus (YFV) transmission1
| AFRICA | CENTRAL AND SOUTH AMERICA | ||
|---|---|---|---|
| Angola Benin Burkina Faso Burundi Cameroon Central African Republic Chad2 Congo, Republic of the Côte d'Ivoire Democratic Republic of the Congo2 | Equatorial Guinea Ethiopia2 Gabon Gambia, The Ghana Guinea Guinea-Bissau Kenya2 Liberia Mali2 | Mauritania2 Niger2 Nigeria Rwanda Senegal Sierra Leone Sudan2 Togo Uganda | Argentina2 Bolivia2 Brazil2 Colombia2 Ecuador2 French Guiana Guyana Panama2 Paraguay Peru2 Suriname Trinidad and Tobago2 Venezuela2 |
1Countries/areas where "a risk of yellow fever transmission is present," as defined by the World Health Organization, are countries or areas where "yellow fever has been reported currently or in the past, plus vectors and animal reservoirs currently exist" (see the current country list within the International Travel and Health publication (Annex 1) at www.who.int/ith/en/index.html![]() ).
).
2These countries are not holoendemic (only a portion of the country has risk of yellow fever transmission). See Maps 3-18 and 3-19 and yellow fever vaccine recommendations (Yellow Fever and Malaria Information, by Country) for details.
Table 3-22. Countries with low potential for exposure to yellow fever virus (YFV)1
| AFRICA |
|---|
| Eritrea2 São Tomé and Príncipe3 Somalia2 Tanzania3 Zambia2 |
1Countries listed in this table are not contained on the official WHO list of countries with risk of YFV transmission (Table 3-21). Therefore, proof of yellow fever vaccination should not be required if traveling from one of these countries to another country with a vaccination entry requirement (unless that country requires proof of yellow fever vaccination from all arriving travelers; see Table 3-24).
2 These countries are classified as "low potential for exposure to YFV" in only some areas; the remaining areas of these countries are classified as having no risk of exposure to YFV.
3 The entire area of these countries is classified as "low potential for exposure to YFV."
RISK FOR TRAVELERS
A traveler's risk for acquiring yellow fever is determined by various factors, including immunization status, location of travel, season, duration of exposure, occupational and recreational activities while traveling, and local rate of virus transmission at the time of travel. Although reported cases of human disease are the principal indicator of disease risk, case reports may be absent because of a low level of transmission, a high level of immunity in the population (because of vaccination, for example), or failure of local surveillance systems to detect cases. This "epidemiologic silence" does not equate to absence of risk and should not lead to travel without the protection provided by vaccination.
YFV transmission in rural West Africa is seasonal, with an elevated risk during the end of the rainy season and the beginning of the dry season (usually July–October). However, YFV may be episodically transmitted by Ae. aegypti even during the dry season in both rural and densely settled urban areas.
The risk for infection in South America is highest during the rainy season (January–May, with a peak incidence in February and March). Given the high level of viremia that may occur in infected humans and the widespread distribution of Ae. aegypti in many towns and cities, South America is at risk for a large-scale urban epidemic.
From 1970 through 2010, a total of 9 cases of yellow fever were reported in unvaccinated travelers from the United States and Europe who traveled to West Africa (5 cases) or South America (4 cases). Eight (88%) of these 9 travelers died. There has been only 1 documented case of yellow fever in a vaccinated traveler. This nonfatal case occurred in a traveler from Spain who visited several West African countries during 1988.
The risk of acquiring yellow fever is difficult to predict because of variations in ecologic determinants of virus transmission. For a 2-week stay, the risks for illness and death due to yellow fever for an unvaccinated traveler traveling to an endemic area in:
- West Africa are 50 per 100,000 and 10 per 100,000, respectively
- South America are 5 per 100,000 and 1 per 100,000, respectively
These estimates are a rough guideline based on the risk to indigenous populations, often during peak transmission season. Thus, these risk estimates may not accurately reflect the true risk to travelers, who may have a different immunity profile, take precautions against getting bitten by mosquitoes, and have less outdoor exposure.
The risk of acquiring yellow fever in South America is lower than that in Africa, because the mosquitoes that transmit the virus between monkeys in the forest canopy in South America do not often come in contact with humans. Additionally, there is a relatively high level of immunity in local residents because of vaccine use, which might reduce the risk of transmission.
CLINICAL PRESENTATION
Asymptomatic or clinically inapparent infection is believed to occur in most people infected with YFV. For people who develop symptomatic illness, the incubation period is typically 3–6 days. The initial illness presents as a nonspecific influenzalike syndrome with sudden onset of fever, chills, headache, backache, myalgias, prostration, nausea, and vomiting. Most patients improve after the initial presentation. After a brief remission of hours to a day, approximately 15% of patients progress to a more serious or toxic form of the disease characterized by jaundice, hemorrhagic symptoms, and eventually shock and multisystem organ failure. The case-fatality ratio for severe cases with hepatorenal dysfunction is 20%–50%.
DIAGNOSIS
The preliminary diagnosis is based on the patient's clinical features, places and dates of travel, and activities. Laboratory diagnosis is best performed by:
- Serologic assays to detect virus-specific IgM and IgG antibodies. Because of cross-reactivity between antibodies raised against other flaviviruses, more specific antibody testing, such as a plaque reduction neutralization test, should be done to confirm the infection.
- Virus isolation or nucleic acid amplification tests performed early in the illness for YFV or yellow fever viral RNA. However, by the time more overt symptoms are recognized, the virus or viral RNA is usually undetectable. Therefore, virus isolation and nucleic acid amplification should not be used for ruling out a diagnosis of yellow fever.
Clinicians should contact their state or local health department or call 800-CDC-INFO (800-232-4636) for assistance with diagnostic testing for yellow fever infections and for questions about antibody response to vaccination.
TREATMENT
Treatment is for symptoms. Rest, fluids, and use of analgesics and antipyretics may relieve symptoms of fever and aching. Care should be taken to avoid certain medications, such as aspirin or nonsteroidal anti-inflammatory drugs, which may increase the risk for bleeding. Infected people should be protected from further mosquito exposure (staying indoors or under a mosquito net) during the first few days of illness, so they do not contribute to the transmission cycle.
PREVENTIVE MEASURES FOR TRAVELERS
Personal Protection Measures
The best way to prevent mosquitoborne diseases, including yellow fever, is to avoid mosquito bites (see Chapter 2, Protection against Mosquitoes, Ticks, and Other Insects and Arthropods).
Vaccine
Yellow fever is preventable by a relatively safe, effective vaccine. All yellow fever vaccines currently manufactured are live-attenuated viral vaccines. YF-Vax, the only yellow fever vaccine licensed for use in the United States, is manufactured by Sanofi Pasteur. Studies comparing the reactogenicity and immunogenicity of various yellow fever vaccines, including those manufactured outside the United States, suggest that there is no significant difference in the reactogenicity or immune response generated by the various vaccines. Thus, people who receive yellow fever vaccines in other countries should be considered protected against yellow fever.
Indications for Use
Yellow fever vaccine is recommended for people aged ≥9 months who are traveling to or living in areas at risk for VFV transmission in South America and Africa. In addition, some countries require proof of yellow fever vaccination for entry. See the Yellow Fever and Malaria Information, by Country section at the end of this chapter for more detailed information on the requirements and recommendations for yellow fever vaccination for specific countries.
Because of the risk of serious adverse events that can occur after yellow fever vaccination, clinicians should only vaccinate people who 1) are at risk of exposure to YFV or 2) require proof of vaccination to enter a country. To further minimize the risk of serious adverse events, clinicians should carefully observe the contraindications and consider the precautions to vaccination before administering yellow fever vaccine (Table 3-23). For additional information, refer to the yellow fever vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) at www.cdc.gov/vaccines/pubs/ACIP-list.htm.
Vaccine Administration
For all eligible people, a single injection of 0.5 mL of reconstituted vaccine should be administered subcutaneously. The International Health Regulations (IHR) published by the World Health Organization (WHO) require revaccination at 10-year intervals.
Vaccine Safety and Adverse Reactions
Common adverse reactions
Reactions to yellow fever vaccine are generally mild; 10%–30% of vaccinees report mild systemic adverse events. Reported events typically include low-grade fever, headache, and myalgias that begin within days after vaccination and last 5–10 days. Approximately 1% of vaccinees temporarily curtail their regular activities because of these reactions.
Severe adverse reactions
Hypersensitivity
Immediate hypersensitivity reactions, characterized by rash, urticaria, bronchospasm, or a combination of these, are uncommon. Anaphylaxis after yellow fever vaccine is reported to occur at a rate of 1.8 cases per 100,000 doses administered.
Yellow fever vaccine–associated neurologic disease (YEL-AND)
YEL-AND represents a conglomerate of different clinical syndromes, including meningoencephalitis, Guillain-Barré syndrome, acute disseminated encephalomyelitis, bulbar palsy, and Bell palsy. Historically, YEL-AND was seen primarily among infants as encephalitis, but more recent reports have been among people of all ages.
The onset of illness for documented cases is 3–28 days after vaccination, and almost all cases were in first-time vaccine recipients. YEL-AND is rarely fatal. The incidence of YEL-AND in the United States is 0.8 per 100,000 doses administered. The rate is higher in people aged ≥60 years, with a rate of 1.6 per 100,000 doses in people aged 60–69 and 2.3 per 100,000 doses in people aged ≥70 years.
Yellow fever vaccine–associated viscerotropic disease (YEL-AVD)
YEL-AVD is a severe illness similar to wild-type disease, with vaccine virus proliferating in multiple organs and often leading to multisystem organ failure and death. Since the initial cases of YEL-AVD were published in 2001, more than 50 confirmed and suspected cases have been reported throughout the world.
YEL-AVD appears to occur after the first dose of yellow fever vaccine, rather than with booster doses. The onset of illness for YEL-AVD cases averaged 3 days (range, 1–8 days) after vaccination. The case-fatality ratio for reported YEL-AVD cases is 65%. The incidence of YEL-AVD in the United States is 0.4 cases per 100,000 doses of vaccine administered. The rate is higher for people aged ≥60 years, with a rate of 1.0 per 100,000 doses in people aged 60–69 years and 2.3 per 100,000 doses in people aged ≥70 years.
Contraindications
Infants younger than 6 months
Yellow fever vaccine is contraindicated for infants aged <6 months. This contraindication was instituted in the late 1960s in response to a high rate of YEL-AND documented in vaccinated young infants (50–400 per 100,000). The mechanism of increased neurovirulence in infants is unknown but may be due to the immaturity of the blood-brain barrier, higher or more prolonged viremia, or immune system immaturity.
Hypersensitivity
Yellow fever vaccine is contraindicated for people with a history of hypersensitivity to any of the vaccine components, including eggs, egg products, chicken proteins, or gelatin. The stopper used in vials of vaccine also contains dry latex rubber, which may cause an allergic reaction.
If vaccination of a person with a questionable history of hypersensitivity to one of the vaccine components is considered essential because of a high risk for acquiring yellow fever, skin testing, as described in the vaccine package insert, should be performed under close medical supervision. If a person has a positive skin test to the vaccine or has a severe egg sensitivity and the vaccination is recommended, desensitization, as described in the package insert, can be performed under direct supervision of a physician experienced in the management of anaphylaxis.
Altered immune status
Thymus disorder
Yellow fever vaccine is contraindicated for people with a thymus disorder that is associated with abnormal immune cell function, such as thymoma or myasthenia gravis. If travel to a yellow fever–endemic area cannot be avoided in a person with a thymus disorder that is associated with abnormal immune cell function, a medical waiver should be provided and counseling on protective measures against mosquito bites should be emphasized. Because there is no evidence of immune dysfunction or increased risk of yellow fever vaccine–associated serious adverse events in people who have undergone incidental surgical removal of their thymus or have had indirect radiation therapy in the distant past, these people can be given yellow fever vaccine if recommended or required.
HIV infection
Yellow fever vaccine is contraindicated for people with AIDS or other clinical manifestations of HIV, including people with CD4 T-lymphocyte values <200/mm3 or <15% of total lymphocytes for children less than <6 years. This recommendation is based on a theoretical increased risk of encephalitis in this population (see HIV infection under the following section, Precautions).
If travel to a yellow fever–endemic area cannot be avoided in a person with severe immune suppression based on CD4 counts (<200/mm3 or <15% total for children less than <6 years) or symptomatic HIV, a medical waiver should be provided, and counseling on protective measures against mosquito bites should be emphasized. See the following section, Precautions, for other HIV-infected people not meeting the above criteria.
Immunodeficiencies (other than thymus disorder or HIV infection)
Yellow fever vaccine is contraindicated for people with primary immunodeficiencies, malignant neoplasms, and transplantation. While there are no data on the use of yellow fever vaccine in these people, they presumably are at increased risk for yellow fever vaccine–associated serious adverse events (see the section in Chapter 8, Immunocompromised Travelers).
If someone with an immunodeficiency cannot avoid travel to a yellow fever–endemic area, a medical waiver should be provided, and counseling on protective measures against mosquito bites should be emphasized.
Immunosuppressive and immunomodulatory therapies
Yellow fever vaccine is contraindicated for people whose immunologic response is either suppressed or modulated by current or recent radiation therapies or drugs. Drugs with known immunosuppressive or immunomodulatory properties include, but are not limited to, high-dose systemic corticosteroids, alkylating drugs, antimetabolites, tumor necrosis factor α inhibitors (such as etanercept), interleukin-1 blocking agents (such as anakinra), or other monoclonal antibodies targeting immune cells (such as rituximab or alemtuzumab). There are no specific data on the use of yellow fever vaccine in people receiving these therapies. However, these people are presumed to be at increased risk for yellow fever vaccine–associated serious adverse events, and the use of live attenuated vaccines is contraindicated in the package insert for most of these therapies (see the section in Chapter 8, Immunocompromised Travelers).
Live viral vaccines should be deferred in people who have discontinued these therapies until immune function has improved. If travel to a yellow fever–endemic area cannot be avoided for someone receiving immunosuppressive or immunomodulatory therapies, a medical waiver should be provided and counseling on protective measures against mosquito bites should be emphasized.
Family members of people with an altered immune status who themselves have no contraindications can receive yellow fever vaccine.
Precautions
Infants aged 6–8 months
Age 6–8 months is a precaution for yellow fever vaccination. Two cases of YEL-AND have been reported among infants aged 6–8 months. In infants <6 months of age, the rates of YEL-AND are significantly elevated (50–400 per 100,000). By 9 months of age, risk for YEL-AND is believed to be substantially lower. ACIP generally recommends that, whenever possible, travel to yellow fever-endemic countries should be postponed or avoided for children aged 6–8 months. If travel is unavoidable, the decision of whether to vaccinate these infants needs to balance the risks of YFV exposure with the risk for adverse events after vaccination.
Adults 60 years of age or older
Age ≥60 years is a precaution for yellow fever vaccination, particularly if this is the first dose of the yellow fever vaccine given. A recent analysis of adverse events passively reported to VAERS from 2000 through 2006 indicates that people aged ≥60 years are at increased risk for any serious adverse event after vaccination, compared with younger people. The rate of serious adverse events in people aged ≥60 years was 8.3 per 100,000 doses distributed, compared with 4.7 per 100,000 for all vaccine recipients. The risk of YEL-AND and YEL-AVD is also increased in this age group, at 1.8 and 1.4 per 100,000 doses, respectively, compared with 0.8 and 0.4 per 100,000 for all vaccine recipients. Given that YEL-AND and YEL-AVD are seen almost exclusively in primary vaccine recipients, more caution should be exercised with older travelers who may be receiving yellow fever vaccine for the first time. If travel is unavoidable, the decision to vaccinate travelers aged ≥60 years needs to weigh the risks and benefits of the vaccination in the context of their destination-specific risk for exposure to YFV.
HIV infection
Asymptomatic HIV infection with CD4 T-lymphocyte values 200–499/mm3 or 15%–24% of total lymphocytes for children aged <6 years is a precaution for yellow fever vaccination (see also the HIV infection in the Contraindications section above). Large prospective, randomized trials have not been performed to adequately address the safety and efficacy of yellow fever vaccine among this group. Several retrospective and prospective studies including approximately 450 people infected with HIV have reported no serious adverse events among patients considered moderately immunosuppressed based on their CD4 counts. However, HIV infection has been associated with a reduced immunologic response to a number of inactivated and live attenuated vaccines, including yellow fever vaccine. The mechanisms for the diminished immune response in HIV-infected people are uncertain but appear to be correlated with HIV RNA levels and CD4 T-cell counts.
Because vaccinating asymptomatic HIV-infected people might be less effective than vaccinating people not infected with HIV, their neutralizing antibody response to vaccination should be measured before travel. Contact the appropriate state health department or the CDC Arboviral Diseases Branch (970-221-6400) to further discuss serologic testing.
If an asymptomatic HIV-infected person with moderate immune suppression (CD4 T-lymphocyte values 200–499/mm3 or 15%–24% of total lymphocytes for children aged <6 years) is traveling to a yellow fever–endemic area, vaccination may be considered. Vaccinated people should be monitored closely after vaccination for evidence of adverse events, and the state health department or CDC should be notified if an adverse event occurs.
If international travel requirements—not risk of yellow fever—are the only reason to vaccinate an HIV-infected person, the person should be excused from immunization and issued a medical waiver to fulfill health regulations. If an asymptomatic HIV-infected person has no evidence of immune suppression based on CD4 counts (CD4 T-lymphocyte values ≥500/mm3 or ≥25% of total lymphocytes for children aged <6 years), yellow fever vaccine can be administered if recommended.
Pregnancy
Pregnancy is a precaution for yellow fever vaccine administration. The safety of yellow fever vaccination during pregnancy has not been studied in a large prospective trial. However, a recent study of women who were vaccinated with yellow fever vaccine early in their pregnancies found no major malformations in their infants. A slight increased risk was noted for minor, mostly skin, malformations in infants. A higher rate of spontaneous abortions in pregnant women receiving the vaccine was reported but not substantiated. The proportion of women vaccinated during pregnancy who develop yellow fever IgG-specific antibodies is variable depending on the study (39% or 98%) and may be correlated with the trimester in which they received the vaccine. Because pregnancy may affect immunologic function, serologic testing can be considered to document a protective immune response to the vaccine.
If travel is unavoidable and the vaccination risks are felt to outweigh the risks of YFV exposure, pregnant women should be excused from immunization and issued a medical waiver to fulfill health regulations. Pregnant women who must travel to areas where YFV exposure is likely should be vaccinated. Although there are no specific data, ACIP recommends that a woman wait 4 weeks after receiving the yellow fever vaccine before conceiving.
Breastfeeding
Breastfeeding is a precaution for yellow fever vaccine administration. Two YEL-AND cases have been reported in exclusively breastfed infants whose mothers were vaccinated with yellow fever vaccine. Both infants were aged <1 month at the time of exposure. Further research is needed to document the risk of potential vaccine exposure through breastfeeding. Until more information is available, yellow fever vaccine should be avoided in breastfeeding women. However, when travel of nursing mothers to a yellow fever–endemic area cannot be avoided or postponed, these women should be vaccinated.
Other Considerations
Chronic medical conditions that may be associated with varying degrees of immune deficit include, but are not limited to, chronic renal disease, chronic liver disease (including hepatitis C), and diabetes mellitus. Because no information is available regarding possible increased adverse events or decreased vaccine efficacy after administration of yellow fever vaccine to patients with these diseases, caution should be used if considering vaccination of such patients. Factors to consider in assessing patients' general level of immune competence include disease severity, duration, clinical stability, complications, and comorbidities.
Simultaneous Administration of Other Vaccines and Drugs
Determination of whether to administer yellow fever vaccine and other immunobiologics simultaneously (administration on the same day but at a different injection site) should be made on the basis of convenience to the traveler in completing the desired vaccinations before travel and on information regarding potential immune interference. No evidence exists that inactivated vaccines interfere with the immune response to yellow fever vaccine. Therefore, inactivated vaccines can be administered either simultaneously or at any time before or after yellow fever vaccination. ACIP recommends that yellow fever vaccine be given at the same time as other live-virus vaccines. Otherwise, the clinician should wait 30 days between vaccinations, as the immune response to one live-virus vaccine might be impaired if administered within 30 days of another live-virus vaccine. Because of the different routes of administration, oral Ty21a typhoid vaccine can be administered simultaneously or at any interval before or after yellow fever vaccine.
Table 3-23. Contraindications and precautions to yellow fever vaccine administration
| CONTRAINDICATIONS | PRECAUTIONS |
|---|---|
|
|
1Symptoms of HIV are classified in 1) Adults and Adolescents, Table 1. CDC. 1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults.MMWR Recomm Rep 1992 Dec 18: 41(RR-17). Available from: www.cdc.gov/mmwr/preview/mmwrhtml/00018871.htm and 2) Panel on Antiretroviral Therapy and Medical Management of HIV-Infected Children. Guidelines for the use of antiretroviral agents in pediatric HIV infection. 2010. Available from: http://aidsinfo.nih.gov/ContentFiles/PediatricGuidelines.pdf ![]()
![]() (PDF). p. 20-2.
(PDF). p. 20-2.
INTERNATIONAL CERTIFICATE OF VACCINATION OR PROPHYLAXIS (ICVP)
The IHRs allow countries to require proof of yellow fever vaccination as a condition of entry for travelers arriving from certain countries, even if only in transit, to prevent importation and indigenous transmission of YFV. Some countries require evidence of vaccination from all entering travelers, which includes direct travel from the United States (Table 3-24). Travelers who arrive in a country with a yellow fever vaccination entry requirement without proof of yellow fever vaccination may be quarantined for up to 6 days, refused entry, or vaccinated on site. A traveler who has a specific contraindication to yellow fever vaccine and who cannot avoid travel to a country requiring vaccination should request a waiver from a physician before embarking on travel (see the Medical Waivers section).
Authorization to Provide Vaccinations and to Validate the ICVP
Under the revised IHR (2005), effective December 15, 2007, all state parties (countries) are required to issue a new ICVP. This is intended to replace the former International Certificate of Vaccination against Yellow Fever (ICV). People who received a yellow fever vaccination after December 15, 2007, must provide proof of vaccination on the new ICVP. If the person received the vaccine before December 15, 2007, the original ICV card is still valid, provided that the vaccination was given <10 years previously. Vaccinees should receive a completed ICVP (Figure 3-01), validated (stamped and signed) with the center's stamp where the vaccine was given (see below). An ICVP must be complete in every detail; if incomplete or inaccurate, it is not valid. Failure to secure validations can cause a traveler to be quarantined, denied entry, or possibly revaccinated at the point of entry to a country. Revaccination at the point of entry is not a recommended option for the traveler.
Clinics may purchase ICVPs, CDC 731 (formerly PHS 731), from the US Government Printing Office (http://bookstore.gpo.gov/![]() , 866-512-1800). The stock number is 017-001-00567-3 for 25 copies and 017-001-00566-5 for 100 copies. This certificate of vaccination is valid for a period of 10 years, beginning 10 days after the date of vaccination. When a booster dose of the vaccine is given within this 10-year period, the certificate is considered valid from the date of revaccination.
, 866-512-1800). The stock number is 017-001-00567-3 for 25 copies and 017-001-00566-5 for 100 copies. This certificate of vaccination is valid for a period of 10 years, beginning 10 days after the date of vaccination. When a booster dose of the vaccine is given within this 10-year period, the certificate is considered valid from the date of revaccination.
People Authorized to Sign the ICVP and Designated Yellow Fever Vaccination Centers
The ICVP must be signed by a medical provider, who may be a licensed physician or a health care worker designated by the physician, supervising the administration of the vaccine (Figure 3-01). A signature stamp is not acceptable. Yellow fever vaccination must be given at a certified center in possession of an official "uniform stamp," which can be used to validate the ICVP.
State health departments are responsible for designating nonfederal yellow fever vaccination centers and issuing uniform stamps to clinicians. Information about the location and hours of yellow fever vaccination centers may be obtained by visiting CDC's website at wwwnc.cdc.gov/travel/yellow-fever-vaccination-clinics-search.aspx.
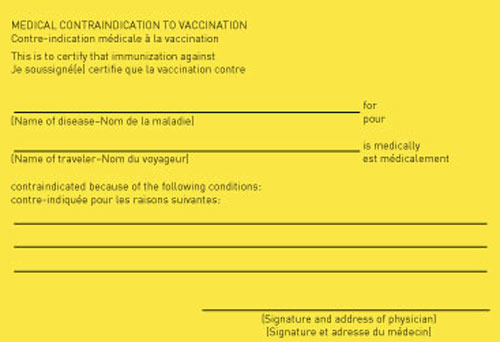
Medical Waivers (Exemptions)
Some countries do not require an ICVP for infants younger than a certain age (<6 months, <9 months, or <1 year of age, depending on the country). Age requirements for vaccination for individual countries can be found in the Yellow Fever and Malaria Information, by Country section in this chapter. For medical contraindications, a physician who has decided to issue a waiver should fill out and sign the Medical Contraindications to Vaccination section of the ICVP (Figure 3-02). The clinician should also do the following:
- Give the traveler a signed and dated exemption letter on the physician's letterhead stationery, clearly stating the contraindications to vaccination and bearing the stamp used by the yellow fever vaccination centers to validate the ICVP.
- Inform the traveler of any increased risk for yellow fever infection associated with nonvaccination and how to minimize this risk by avoiding mosquito bites.
Reasons other than medical contraindications are not acceptable for exemption from vaccination. The traveler should be advised that issuance of a waiver does not guarantee its acceptance by the destination country. On arrival at the destination, the traveler may be faced with quarantine, refusal of entry, or vaccination on site. To improve the likelihood that the waiver will be accepted at the destination country, clinicians can suggest that the traveler take the following additional measures before beginning travel:
- Obtain specific and authoritative advice from the embassy or consulate of the destination country or countries.
- Request documentation of requirements for waivers from embassies or consulates and retain these along with the completed Medical Contraindication to Vaccination section of the ICVP.
Table 3-24. Countries that require proof of yellow fever vaccination from all arriving travelers1
| Angola Benin Burkina Faso Burundi Cameroon Central African Republic Congo, Repubic of the Côte d'Ivoire Democratic Republic of Congo French Guiana | Gabon Ghana Guinea-Bissau Liberia Mali Niger Rwanda São Tomé and Príncipe Sierra Leone Togo |
1 Country requirements for yellow fever vaccination are subject to change at any time; therefore, CDC encourages travelers to check with the destination country's embassy or consulate before departure.
Figure 3-01. Example International Certificate of Vaccination or Prophylaxis (ICVP)
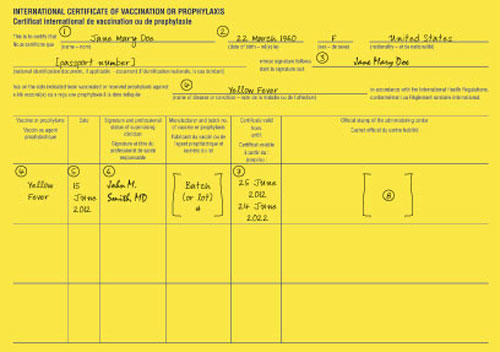
(2, 5, 7) All dates should be entered with the day in numerals, followed by the month in letters, then the year. For example: in the above example, the patient's date of birth is 22 March 1960.
(3) This space is for the patient's signature.
(4) For a yellow fever vaccination, 'Yellow Fever' should be written in both spaces. Should the ICVP be used for a required vaccination or prophylaxis against another disease or condition (following an amendment to the International Health Regulations or by recommendation of WHO), that disease or condition should be written in this space. Other vaccinations may be listed on the other side.
(5) The date on which the vaccination is given should be entered as shown above.
(6) A handwritten signature of the clinician—either the stamp holder or another health care provider authorized by the stamp holder—administering or supervising the administration of the vaccine (or prophylaxis) should appear in this box. A signature stamp is not acceptable.
(7) The certificate of yellow fever vaccination is valid for 10 years, beginning 10 days after the date of primary vaccination. The ending date for a valid vaccination recorded on the ICVP is 1 calendar day prior to the calendar day on which the vaccine became valid. For example, a vaccination given on 15 June 2012 will be valid on 25 June 2012 and will expire on 24 June 2022. In the case of revaccination, the certificate of yellow fever vaccination is valid immediately if documentation exists on an ICVP demonstrating that the previous yellow fever vaccination was given within the last 10 years.
(8) The Uniform Stamp of the vaccinating center should appear in this box.
Figure 3-02. Medical Contraindication to Vaccination section of the International Certificate of Vaccination or Prophylaxis (ICVP)
REQUIREMENTS VERSUS RECOMMENDATIONS
Country entry requirements for proof of yellow fever vaccination under the IHRs are different from CDC's recommendations. Yellow fever vaccine entry requirements are established by countries to prevent the importation and transmission of YFV and are allowed under the IHRs. Travelers must comply with these to enter the country, unless they have been issued a medical waiver. Certain countries require vaccination from travelers arriving from all countries, while some countries require vaccination only for travelers coming from "a country with risk of yellow fever transmission" (see the Yellow Fever and Malaria Information, by Country section in this chapter). WHO defines those areas "with risk of yellow fever transmission" as countries or areas where yellow fever has been reported currently or in the past, plus where vectors and animal reservoirs exist. Country requirements are subject to change at any time; therefore, CDC encourages travelers to check with the appropriate embassy or consulate before departure.
The information in the section on yellow fever vaccine recommendations is advice given by CDC to prevent yellow fever infections among travelers. Recommendations are subject to change at any time if disease conditions change; therefore, CDC encourages travelers to check the destination pages for up-to-date vaccine information and to check for relevant travel notices on the CDC website before departure (www.cdc.gov/travel).
NEW CHANGES TO YELLOW FEVER RISK CLASSIFICATION AND CDC VACCINE RECOMMENDATIONS
CDC, WHO, and other yellow fever experts recently completed a comprehensive review of available data and revised the criteria and global maps designating the risk of YFV transmission. The new criteria establish 4 categories of risk for YFV transmission that apply to all geographic areas: endemic, transitional, low potential for exposure, and no risk.
Yellow fever vaccination is recommended for travel to endemic and transitional areas. Although vaccination is generally not recommended for travel to areas with low potential for exposure, it might be considered for a small subset of travelers whose itinerary could place them at increased risk for exposure to YFV (such as prolonged travel, heavy exposure to mosquitoes, or inability to avoid mosquito bites).
Based on the revised criteria for yellow fever risk classification, the current maps (Maps 3-18 and 3-19) and country-specific information (see the Yellow Fever and Malaria Information, by Country later in this chapter) designate 3 levels of yellow fever vaccine recommendations: recommended, generally not recommended, and not recommended. Note: The revised yellow fever Maps 3-18 and 3-19 now depict vaccination recommendations rather than yellow fever risk.
Countries that only contain areas with low potential for exposure to YFV (Table 3-22) are not included on the official WHO list of countries with risk of YFV transmission (Table 3-21). Therefore, proof of yellow fever vaccination should not be required if traveling from a country with low potential for exposure to YFV to a country with a vaccination entry requirement (unless that country requires proof of yellow fever vaccination from all arriving travelers; see Table 3-24).
Map 3-18. Yellow fever vaccine recommendations in Africa, 2010
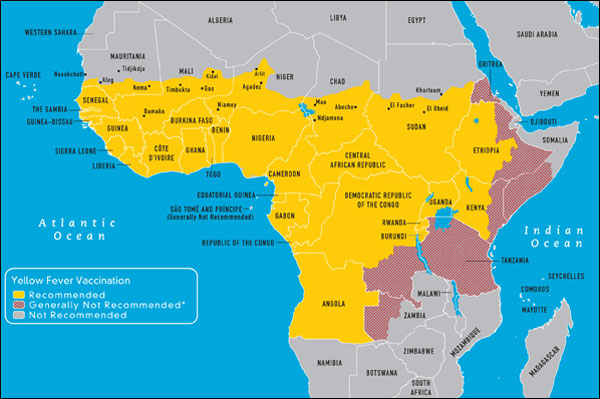
View Larger Map PDF Version (printable) ![]()
*Yellow fever (YF) vaccination is generally not recommended in areas where there is low potential for YF virus exposure. However, vaccination might be considered for a small subset of travelers to these areas who are at increased risk for exposure to YF virus because of prolonged travel, heavy exposure to mosquitoes, or inability to avoid mosquito bites. Consideration for vaccination of any traveler must take into account the traveler's risk of being infected with YF virus, country entry requirements, and individual risk factors for serious vaccine-associated adverse events (e.g., age, immune status).
Map 3-19. Yellow fever vaccine recommendations in the Americas, 2010
*Update: For the most current yellow fever vaccine recommendations for Brazil, see CDC Yellow Fever Recommendations for Brazil.

*Yellow fever (YF) vaccination is generally not recommended in areas where there is low potential for YF virus exposure. However, vaccination might be considered for a small subset of travelers to these areas who are at increased risk for exposure to YF virus because of prolonged travel, heavy exposure to mosquitoes, or inability to avoid mosquito bites. Consideration for vaccination of any traveler must take into account the traveler's risk of being infected with YF virus, country entry requirements, and individual risk factors for serious vaccine-associated adverse events (e.g., age, immune status).
VACCINATION FOR TRAVEL ON MILITARY ORDERS
Because military requirements may exceed those indicated in this publication, any person who plans to travel on military orders (civilians and military personnel) should contact the nearest military medical facility to determine the requirements for his or her trip.
BIBLIOGRAPHY
- Barwick R. History of thymoma and yellow fever vaccination. Lancet. 2004 Sep 11–17;364(9438):936.
- Cavalcanti DP, Salomao MA, Lopez-Camelo J, Pessoto MA. Early exposure to yellow fever vaccine during pregnancy. Trop Med Int Health. 2007 Jul;12(7): 833–7.
- CDC. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010.
- CDC. Transmission of yellow fever vaccine virus through breast-feeding—Brazil, 2009. MMWR Morb Mortal Wkly Rep. 2010 Feb 12;59(5):130–2.
- Fletcher MA, Fabre P, Debois H, Saliou P. Vaccines administered simultaneously: directions for new combination vaccines based on an historical review of the literature. Int J Infect Dis. 2004 Nov;8(6): 328–38.
- Hayes EB. Acute viscerotropic disease following vaccination against yellow fever. Trans R Soc Trop Med Hyg. 2007 Oct;101(10):967–71.
- Lindsey NP, Schroeder BA, Miller ER, Braun MM, Hinckley AF, Marano N, et al. Adverse event reports following yellow fever vaccination. Vaccine. 2008 Nov 11;26(48):6077–82.
- McMahon AW, Eidex RB, Marfin AA, Russell M, Sejvar JJ, Markoff L, et al. Neurologic disease associated with 17D-204 yellow fever vaccination: a report of 15 cases. Vaccine. 2007 Feb 26;25(10):1727–34.
- Monath TP, Cetron MS. Prevention of yellow fever in people traveling to the tropics. Clin Infect Dis. 2002 May 15;34(10):1369–78.
- Monath TP, Nichols R, Archambault WT, Moore L, Marchesani R, Tian J, et al. Comparative safety and immunogenicity of two yellow fever 17D vaccines (ARILVAX and YF-VAX) in a phase III multicenter, double-blind clinical trial. Am J Trop Med Hyg. 2002 May;66(5):533–41.
- Monath TP, Teuwen D, Cetron MS. Yellow fever vaccine. In: Plotkin S, Orenstein WA, Offit PA, editors. Vaccines. 5th ed. Philadelphia: WB Saunders; 2008. p. 959–1055.
- Nasidi A, Monath TP, Vandenberg J, Tomori O, Calisher CH, Hurtgen X, et al. Yellow fever vaccination and pregnancy: a four-year prospective study. Trans R Soc Trop Med Hyg. 1993 May–Jun;87(3):337–9.
- Nishioka SD, Nunes-Araujo FRF, Pires WP, Silva FA, Costa HL. Yellow fever vaccination during pregnancy and spontaneous abortion: a case-control study. Trop Med Int Health. 1998 Jan;3(1):29–33.
- Pan American Health Organization. Yellow fever in Paraguay: mobilization continues. 2008 [cited 2010 Oct 19]. Available from: http://www.paho.org/English/ad/dpc/cd/eid-eer-2008-02-25.htm
 .
. - Staples JE, Gershman M, Fischer M. Yellow fever vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010 Jul 30;59(RR-7):1–27.
- Suzano CES, Amaral E, Sato HK, Papaiordanou PM, Fever CGY. The effects of yellow fever immunization (17DD) inadvertently used in early pregnancy during a mass campaign in Brazil. Vaccine. 2006 Feb 27;24(9):1421–6.
- Tomori O. Yellow fever: the recurring plague. Crit Rev Clin Lab Sci. 2004;41(4):391–427.
- Whittembury A, Ramirez G, Hernandez H, Ropero AM, Waterman S, Ticona M, et al. Viscerotropic disease following yellow fever vaccination in Peru. Vaccine. 2009 Oct 9;27(43):5974–81.
- World Health Organization. International Health Regulations, 2005. 2008 [cited 2010 Oct 19]. Available from: http://whqlibdoc.who.int/publications/2008/9789241580410_eng.pdf

 .
. - 20 World Health Organization. Yellow fever vaccine. WHO position paper. Wkly Epidemiol Rec. 2003 Oct 3;78(40):349–59.
